Chiropractic Treatment


Physical Medicine Rehabilitation; Therapeutic Physiotherapy Modalities:
Ultrasound (Diathermy) Modality
Ultrasound Diathermy: An adjunctive therapeutic physiotherapy modality that assists with perceived somatic pain, post-traumatic soft tissue injury and joint dysfunction including but not limited to a variety of musculoskeletal conditions, tenosynovitis, bursitis, periarthritis and osteoarthritis.
Ultrasound (Ultrasonic): is an acoustic vibration above frequencies unavailable to the human ear that are able to deeply penetrate into the layers of musculoskeletal tissues.
Diathermy: a method of therapeutic physiotherapy that involves generating local heat in body tissues by high frequency electromagnetic currents.
Summary of Effects: Ultrasound Diathermy Modality generates deep therapeutic heat into the musculoskeletal tissues along with other non-thermal biologic effects: temporarily blocks peripheral nerve impulses (small C-fibers), improves hypertonicity of musculoskeletal spams, alters spinal reflexes, increase the local metabolic rate, increase peripheral arterial blood flow and increase membrane permeability. Additional benefits, viz., Histamine Release, Antisepsis, Analgesia, Clearing Agent (edema with pulsed mode), Chemical Effects, Microdestruction (spurs, calcified hematomas, etcetera), Tissue Alteration (reduction of tonicity of musculoskeletal soft tissue accompanied with the breakdown of collagen fibrils of scar tissue) and Micromassage (deep penetration, fine vibratory action and high frequency).
Interferential Stimulation Modality
Interferential Stimulation Therapeutic Modality involve medium-frequency alternating sine waves which range between 1,000 and 10,000 Hz.
Ideal for: pain (trigger endorphin and enkephalin production), reduction of hypertonic tissue integrity, improvement of hypotonic tissue integrity, swelling | effusion (increased circulation), stimulation of intact motor neurons, stimulation of striated muscle tissue (muscle re-education) and Nerve Block | 4000 Hz | Wedensky Inhibition.
Ultrasound Modality + Interferential Modality Combination
The principal purpose of the combination of: Ultrasound (Diathermy) Modality with that of the Interferential Stimulation Modality is to overcome skin resistance to attain deeper musculoskeletal penetration with more efficacious simulation along with muscle contraction | tetany; also, additional value with the location of and treatment of musculocutaneous trigger points. The conjoined therapeutic benefits and the description thereof are listed above under: Ultrasound (Diathermy) Modality and Interferential Stimulation Modality.
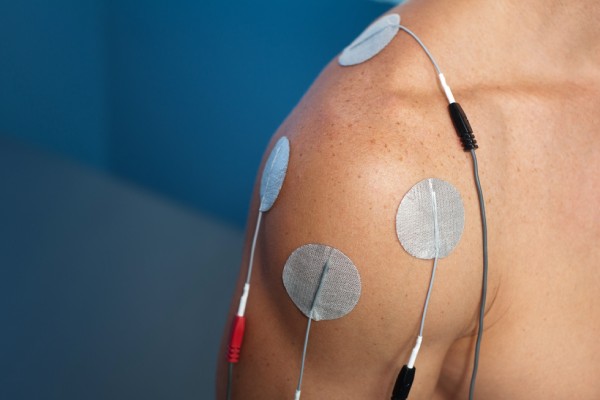
Electric Muscle Stimulation Modality
Any procedure or device that attempts to stimulate muscle tissue with electricity falls under the electric muscle stimulation general category. A modality which stimulates innervated muscles to trigger a contraction independent of the muscles neurologic innervation and be of a tetanic nature. Objectives of electric muscle stimulation is: to reduce the intensity of hypertonic tissue integrity (spastic), to improve the integrity of hypotonic tissue integrity (atrophy), to therapeutically exercise weak musculature (re-educate) and to potentially employ a diagnostic evaluation to determine the degree and | or severity of dysfunction | degeneration.
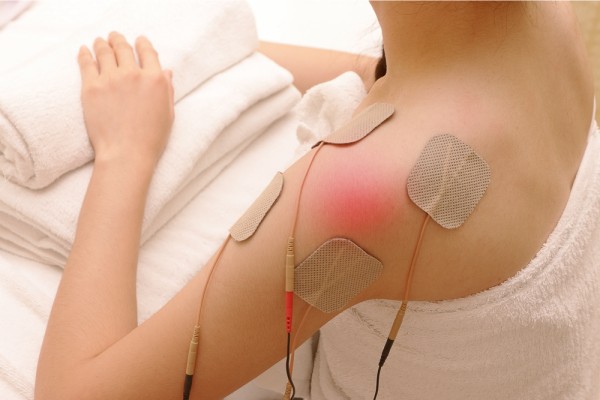
Transcutaneous Electric Nerve Stimulation Modality
A TENS device modality produces an electrical current that passes through the skin; the purpose of this technology is to provide sensory (afferent) stimulation not motor (efferent) stimulation. This technology is a viable alternative to other devices that stimulate motor function that prompt a muscle contraction which may aggravate the patient’s condition; TENS pain control settings typically range from approximately: 70 – 150 pps. The pain modulation of the TENS technology last while the unit is on; once the unit is off, the posttherapy effects will likely be de minimis. The TENS technology is intended for a wide range of pain related conditions, even where pain is qualitatively characterized as: moderate, severe or even intractable.
Hydrotherapy (Moist Heat) Modality
The therapeutic use of moist heat for and with a musculoskeletal injury condition will act as an analgesic (capable of reducing the perception of pain) while potentially inducing a soothing, a calming effect; will increase the local metabolism; will have a sedating effect of the sensory nerve which will trigger enkephalin production, an endogenous neurotransmitter that binds to specific pain related opiate receptors sites; will give rise to the release of histamine or histamine-like substances that bring about arteriolar dilatation (with and from the increase in temperature of the applied therapeutic heat) which will increase the capillary flow and capillary pressure. The increased capillary pressure will yield localized edema where the increased capillary flow will yield increased supply of oxygen, nutrients, antibodies, leukocytes and phagocytosis accompanied with the increased purging of post-traumatic cellular metabolites and the therapeutic heat diffusion.
Cryotherapy Modality
Local Cryotherapy Effects: The therapeutic use of cold for and with a musculoskeletal injury condition will reduce nerve conduction velocities in both motor and sensory fibers (conduction can and will be eliminated within a temperature range of approximately 50 degrees - 59 degrees Fahrenheit); will result in analgesia (absence of pain) as a result of the decrease in the excitability of the muscle afferents; will reduce cell metabolism; will result in localized vasoconstriction; will reduce cellular exudates; will reduce tissue spasticity as a direct result of the decrease in the excitability of muscle afferents, and also; will reduce capillary blood pressure, increase pressure for approximately 4-8 minutes and reduce the pulse.
General Cryotherapy Effects: The therapeutic use of cold for and with a musculoskeletal injury condition will reduce muscle fatigue; will yield an increased respiratory rate: hyperpnea); will produce an increase in the heart rate: tachycardia; and will increase the production of white blood cells: leukocytosis.
The therapeutic cryotherapy modality may be implemented and | or applied, viz., by way of: cold packs, immersion, ice, whirlpools, cryotherapy units and vapocoolant sprays.
Manual Therapy Technique Modality
Manual Therapy Technique Modality include but is not limited to therapeutic and manual soft tissue mobilization and release, connective tissue mobilization and release, trigger point procedures, therapeutic massage, passive ranges of motion, manual traction and joint - myofascial mobilization and release.
The therapeutic benefits include improved and reduced soft tissue pain, restriction, swelling, effusion, inflammation; improved joint ranges of motion, improved and reduced hypertonic tissue integrity (spastic). Manual Therapy Technique Modality may induce therapeutic relaxation thus not only improving contractile soft tissue extensibility but also improving non-contractile soft tissue extensibility.
Manual Therapy Technique Modality is ideal for individuals who present themselves with pain, soft tissue swelling, muscle spasms, restricted ranges of motion, soft tissue adhesions - scar tissue and | or aberrantly contracted soft tissues.
Therapeutic Active Rehabilitative Procedures
Therapeutic Procedures (isotonic | isometric therapeutic activities) support and improve the development of range of motion, flexibility, endurance and strength with and during the physiologic phases of soft tissue healing and rehabilitation, listed below:
- Acute Inflammatory Phase;
- Repair and Regeneration Phase;
- Remodeling and Rehabilitation Phase.
Kinetic Active Rehabilitative Procedures
Kinetic Procedures (isokinetic therapeutic activities) support and improve the development of functional performance with direct and dynamic isokinetic therapeutic activities with and during the physiologic phases of soft tissue healing and rehabilitation processes, listed below:
- Acute Inflammatory Phase;
- Repair and Regeneration Phase;
- Remodeling and Rehabilitation Phase.
Neuromuscular Re-education Modality
Neuromuscular re-education of movement, balance, coordination, kinesthetic sense, posture, and | or proprioception for sitting and | or standing activities. Neuromuscular re-education and movement training require an understanding of the relationship between the stabilization of muscles, the mobilization of muscles and the proper sequence | ideal biomechanical motion patterns for apposite performance and function whether with activities of daily living, occupational activities or sport specific physical performance. With these approaches, prescribed tasks are simplified into their most simple component | function with its single-joint movement pattern. This pattern of component | function is properly biomechanically aligned with breathing and muscle stabilization utilizing manual or mechanical assistance. As this specific single joint component | function becomes more improved | progressed and stable the prescribed neuromuscular re-education modalities will graduate with the level of complexity, the level of difficulty with, by and from: Multiple-Joint | Compound Joint Movements; Circular and | or Diagonal Motions (less emphasis of linear motions); Proprioceptive Variations with less stable, less familiar surfaces with or without eyes open – eye closed progressions; Progressive and Non-Progressive Resistance Patterns and integration of dynamic techniques (variable speeds and durations). Neuromuscular re-education and movement training including: one-to-one instruction, motion and task modeling, tactile cuing, bracing, visual aids, balance boards, a variety of devices with a variety of loads and | or weights, TheraBand devices, etcetera. imagery, audiovisual aids, pressure biofeedback, EMG, assistive training environments such as Pilates or Gyrotonic, balance boards, dumbbells, and other devices. Mastery of a desired skill whether mental, physical and | or functional: unconscious incompetence; conscious incompetence; conscious competence; unconscious competence (mastery of desired skill) where as to improve the odds of a safe, sustainable and injury resistant status.
Proprioceptive Neuromuscular Facilitation (PNF)
Proprioceptive Neuromuscular Facilitation (PNF) are specialized stretching maneuvers designated to promote neuromuscular responses through proprioceptor stimulation. The prime goal is to lessen sensory activity through spinal reflexes to (in effect) relax muscles to be stretched, i.e., relaxation of the targeted muscle being stretched (agonist muscle) with, by, and from the voluntary concentric contraction of the targeted muscles antagonist.
Proprioceptive Neuromuscular Facilitation (PNF) is advantageous for the following: spasms, joint adhesions, deranged articular cartilage, contractures, taut capsules and fibrosis fixations (various end-feel soft-tissue abnormalities).
Proprioceptive Neuromuscular Facilitation (PNF): Contract- Relax PNF Technique; Hold-Relax PNF Technique; Slow-Reversal PNF Hold-Relax Technique; Applied PNF Oscillation.
Neuromuscular re-education of movement, balance, coordination, kinesthetic sense, posture, and | or proprioception for sitting and | or standing activities. Neuromuscular re-education and movement training require an understanding of the relationship between the stabilization of muscles, the mobilization of muscles and the proper sequence | ideal biomechanical motion patterns for apposite performance and function whether with activities of daily living, occupational activities or sport specific physical performance. With these approaches, prescribed tasks are simplified into their most simple component | function with its single-joint movement pattern. This pattern of component | function is properly biomechanically aligned with breathing and muscle stabilization utilizing manual or mechanical assistance. As this specific single joint component | function becomes more improved | progressed and stable the prescribed neuromuscular re-education modalities will graduate with the level of complexity, the level of difficulty with, by and from: Multiple-Joint | Compound Joint Movements; Circular and | or Diagonal Motions (less emphasis of linear motions); Proprioceptive Variations with less stable, less familiar surfaces with or without eyes open – eye closed progressions; Progressive and Non-Progressive Resistance Patterns and integration of dynamic techniques (variable speeds and durations). Neuromuscular re-education and movement training including: one-to-one instruction, motion and task modeling, tactile cuing, bracing, visual aids, balance boards, a variety of devices with a variety of loads and | or weights, TheraBand devices, etcetera. Mastery of a desired skill whether mental, physical and | or functional: unconscious incompetence; conscious incompetence; conscious competence; unconscious competence (mastery of desired skill) where as to improve the odds of a safe, sustainable and injury resistant status.
Therapeutic Gait Training Modality
Therapeutic Gait Training Modality may be medically appropriate and indicated for individuals whose ambulation abilities (walking and gait abilities) have been impaired by muscular, neurological and | or skeletal trauma or abnormalities. The therapeutic goal is to attempt to restore the quality of ambulation through and by prescribed therapeutic activities that in effect improve musculoskeletal | neurological dysfunction so as to be able to safely and proficiently ambulate. This therapeutic modality may be employed on even or uneven surfaces or during simulated stair and step climbing activities.
Therapeutic Gait Training Modality may be medically appropriate and indicated for individuals who experience musculoskeletal trauma whether from or by an accident and injury or surgery and that require gait training re-education. This may also be beneficial for individuals who require the use of walking aids, i.e., crutches, a cane or a walker.
Therapeutic Gait Training Modality is not medically necessary if the individual’s quality of ambulation is not expected to improve.
Functional Capacity Evaluation
Functional capacity evaluation (Wikipedia),
A functional capacity evaluation (FCE) is set of tests, practices and observations that are combined to determine the ability of the evaluated person to function in a variety of circumstances, most often employment, in an objective manner. Physicians change diagnoses based on FCEs.[1] They are also required by insurers in when an insured person applies for disability payments or a disability pension in the case of permanent disability.
Purpose
An FCE can be used to determine fitness to work following an extended period of medical leave. If an employee is unable to return to work, the FCE provides information on prognosis, and occupational rehabilitation measures that may be possible. An FCE can also be used to help identify changes to employee workload, or modifications to working conditions such as ergonomic measures, that the employer may be able to undertake in an effort to accommodate an employee with a disability or medical condition. FCEs are needed to determine if an employee is able to resume working in a capacity "commensurate with his or her skills or abilities"[2] before the disability or medical condition was diagnosed. An FCE involves assessments made by one or more medical doctors. There are two types of FCE used by the United States Social Security Administration: the Mental Functional Capacity Evaluation (MFCE) that measures emotional and mental capacity, and the Physical Functional Capacity Evaluation (PFCE) that measures physical functioning.[2]
Studies have been undertaken to assess the accuracy of FCEs in predicting the longterm outcomes for patients, both in terms of returning to work, and in probability of permanent disability. Questions that have been raised include how to identify medical and societal variables in predicting disability.[3]
FCEs may be required by law for some employers before an employee can return to work, as well as by insurers before insurance payments can be made. FCEs are also used to determine eligibility for disability insurance, or pension eligibility in the event that an employee is permanently unable to return to work. The United States Social Security Administration has its own FCE, called the Assessment of Disability. A newer FCE model is the World Health Organization's International Classification of Functioning, Disability and Health.
During Most FCEs, the following measurements are also taken:
- Lifting power
- Push and pull power
- How long one can stand or walk
- Flexibility and reaching
- Grasping and holding capabilities
- Bending capabilities
- Balance capabilities[4]
Metabolic Equivalents (METs)
Functional capacity can also be expressed as "METs" and can be used as a reliable predictor of future cardiac events.[5] One MET is defined as the amount of oxygen consumed while sitting at rest, and is equal to 3.5 ml oxygen per kilogram body weight per minute. In other words, a means of expressing energy cost of physical activity as a multiple of the resting rate.[6] For instance; walking on level ground at about 6 km/h or carrying groceries up a flight of stairs expends about 4 METs of activity. Generally, >7 METs of activity tolerance is considered excellent while <4 is considered poor for surgical candidates. Determining one's functional capacity can elucidate the degree of surgical risk one might undertake for procedures that risk blood loss, intravascular fluid shifts, etc. and may tax an already strained cardiovascular system.[5]
References
1. Jump up ^ Wind, Haje (October 2009). "Effect of Functional Capacity Evaluation information on the judgment of physicians about physical work ability in the context of disability claims". Int Arch Occup Environ Health. 82 (9): 1087–96. doi:10.1007/s00420-009-0423-8. PMC 2746897 . PMID 19458959.
2. ^ Jump up to: a b Irmo Marini, Mark Stebnicki, ed. (2008). The Professional Counselor's Desk Reference. Springer Publishing Company. p. 519. ISBN 9780826115478.
3. Jump up ^ Chen, M.D., Joseph J. (2007). "Functional Capacity Evaluation and Disability". The Iowa Orthopaedic Journal. 27: 121–127. PMC 2150654 . PMID 17907444.
4. Jump up ^ "FCE Fairfax VA |Woodbridge VA | Silver Spring MD". www.dynamicrehabtherapy.com. Retrieved 2016-04-04.
5. ^ Jump up to: a b Whinney, Christopher M. "Perioperative Evaluation". Cleveland Clinic. Retrieved 2014-01-29.
6. Jump up ^ Jetté, M.; Sidney, K.; Blümchen, G. (August 1990). "Metabolic Equivalents (METS) in Exercise Testing, Exercise Prescription, and Evaluation of Functional Capacity". Clinical Cardiology. Wiley-Blackwell. 13 (8): 555–565. doi:10.1002/clc.4960130809. Retrieved 2014-01-29.
Physical Performance Evaluation
Physical Performance Evaluation
Individuals preparing to return to work if they have experienced extended time away from work due to a work injury may qualify for and benefit from a Physical Performance Evaluation. The Physical Performance Evaluation is an examination of a person's physical ability to perform work activities and to establish his | her PDL (Physical Demand Level).
To evaluate:
- Balance;
- Dexterity;
- Fine-motor coordination;
- Endurance | stamina;
- Dynamic strength (push | pull | lift |carry);
- Varying occupational: kneel, squat, stoop, sit and stand);
- Mobility (step, climb, walk, and crawl);
Once the PDL is formally established, it will be compared with that his | her required PDL for consideration of return to gainful employment, treatment and | or return to work recommendations will ensue thereafter. Also, for individuals exploring an alternate work setting after an injury, the Physical Performance Evaluation may prove useful for and with establishing guidelines | parameters for vocational evaluation for retraining.
Work Readiness Programs
Work Conditioning and Work Hardening Programs:
Injured workers who have participated with a reasonable course of physical medicine rehabilitation | therapy and who are still experiencing physical | functional deficiencies may require participation in a work readiness program: work conditioning and | or work hardening programs. For such injured workers, it’s appropriate for them to participate with either a FCE (Functional Capacity Evaluation) or a PPE (physical performance examination) to establish their PDL (Physical Demand Level). If the injured worker’s PDL falls short to their required PDL (what’s required to return to unrestricted work duties and functions) they may qualify for and greatly benefit from participation with a work readiness program. A work readiness program focuses on a full body approach with intensive conditioning activities combined with work simulation tasks which should advance the injured worker’s PDL to ensure the injured worker will be able to return to unrestricted gainful employment.
Work Conditioning:
A rigorous, goal-oriented conditioning program intended to improve and restore musculoskeletal and neuromuscular function including but not limited to: stamina, ROM, body mechanics, physical tolerance, independent pain management, technique, strength, safety, cardiovascular endurance, power, joint mobility, motor control, and other functional abilities. The principal objective of a single disciplinary Work Conditioning Program is to safely restore physical | functional capacity and ensure the injured worker is afforded an opportunity to attain a pre-injury job status for a successful RTW.
Work Hardening:
An individualized, highly structured, goal-oriented multidisciplinary work readiness program intended to return the employee to unrestricted gainful employments. The work hardening programs utilizes actual or simulated work tasks while therapeutically | occupationally addressing and restoring physical, functional, and vocational roles. Similarly, work hardening focuses on: stamina, ROM, body mechanics, physical tolerance, independent pain management, technique, strength, safety, cardiovascular endurance, power, joint mobility, motor control, other functional abilities as well as the injured worker’s behaviors. The prime objective of a multidisciplinary Work Hardening Program is to restore physical | functional capacity and safely graduate their present PDL to their required PDL so that they may successfully RTW (return to work).
Telephonic healthcare-related consultations are available for the residents of the State of Nevada, the State of Louisiana and the State of Texas.
Call to schedule a telephonic (healthcare-related) consultation with Dr. Patrick R.E. Davis, Chiropractic Physician.